Obsessive-Compulsive Disorder (OCD) is a mental health condition marked by persistent, intrusive thoughts (obsessions) and repetitive behaviors or mental rituals (compulsions). These intrusive thoughts and compulsive actions can substantially disrupt an individual’s daily activities, relationships, and overall mental and emotional health. OCD is more than just being neat or organized. It involves intrusive thoughts that cause anxiety or distress and the need to perform certain rituals or behaviors to alleviate that distress temporarily. These rituals are often time-consuming and can hinder the individual’s ability to function effectively
Common Symptoms of OCD
The symptoms of OCD can vary widely from person to person, but some common manifestations include:
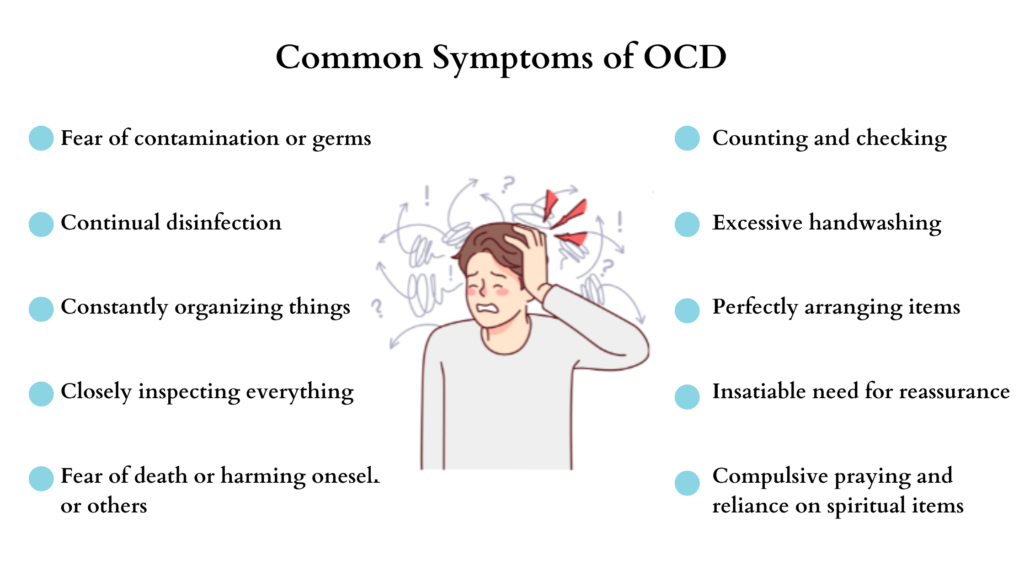
1. Obsessions: These are intrusive and unwanted thoughts, images, or urges that repeatedly occur in a person’s mind. They can be distressing and cause significant anxiety. Common obsessions include fears of contamination, doubts, forbidden thoughts or images, and a need for symmetry or exactness.
2. Compulsions: The provided content discusses repetitive behaviors and mental acts associated with Obsessive-Compulsive Disorder (OCD). Individuals with OCD often feel compelled to engage in these behaviors as a response to their obsessions. These compulsions are typically performed in an effort to alleviate or diminish feelings of anxiety or distress. Examples of common compulsions include excessive hand washing, checking, arranging or counting objects, and repeating specific words or phrases.
3. Impact on daily life: OCD symptoms can significantly impact a person’s daily functioning, relationships, and overall quality of life. Individuals may spend hours each day engaging in compulsions, which can lead to difficulties at work, school, or in personal relationships.
Causes and Risk Factors of OCD
The exact cause of OCD is not yet fully understood. However, research suggests that a combination of genetic, biological, and environmental factors may contribute to its development.
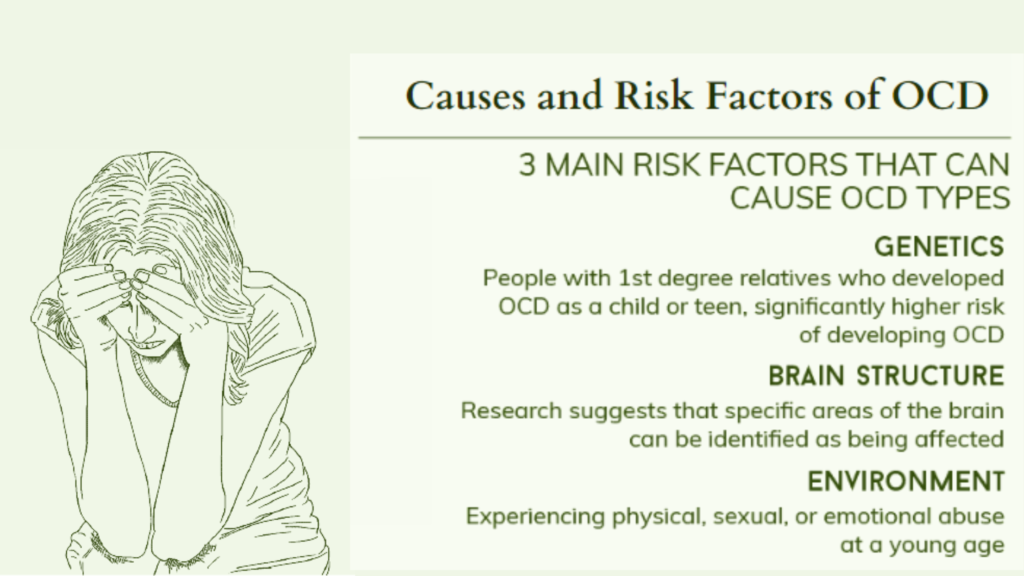
1. Genetic factors: There is some indication that obsessive-compulsive disorder (OCD) may have a hereditary component. A familial connection has been observed, with a heightened likelihood of developing the disorder if a family member, such as a parent or sibling, has been diagnosed with OCD.
2. Brain chemistry and structure: Imbalances in certain chemicals in the brain, such as serotonin, may play a role in the development of OCD. Additionally, abnormalities in certain brain regions involved in decision-making, planning, and impulse control have been observed in individuals with OCD.
3. Environmental factors: Traumatic life events, such as abuse or loss, may trigger the onset of OCD in some individuals. Stressful situations and significant life changes can also exacerbate symptoms.
Diagnosing OCD: How is it Done?
Identifying obsessive-compulsive disorder (OCD) requires a thorough evaluation performed by a qualified mental health professional. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) outlines specific criteria for the diagnosis of OCD.
1. Clinical interview: The mental health professional will conduct a detailed interview to gather information about the individual’s symptoms, their duration, and their impact on daily life.
2. Assessment of obsessions and compulsions: The clinician will assess the nature and severity of the obsessions and compulsions, as well as any associated distress or impairment.
3. Rule out other conditions: It is essential to rule out other mental health conditions that may present with similar symptoms, such as anxiety disorders or hoarding disorders.
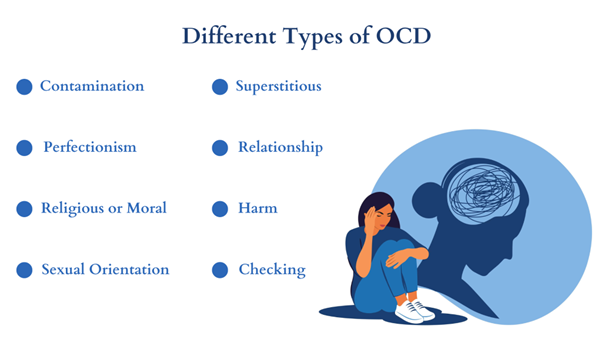
Different Types of OCD
OCD can manifest in different ways, and individuals may experience a range of obsessions and compulsions. Here are some common types of OCD:
1. Contamination OCD
Individuals with contamination OCD have an excessive fear of germs, dirt, or contamination. They may engage in excessive hand washing, avoid touching certain objects, or avoid public places.
2. Harm OCD
This subtype involves intrusive thoughts or fears of causing harm to oneself or others. Individuals may have thoughts of violence, accidents, or unintentional harm and may engage in rituals to prevent these events from occurring.
3. Symmetry OCD
People with symmetry OCD have a strong need for order, symmetry, or exactness. They may spend excessive time arranging objects, aligning items perfectly, or needing things to be “just right.”
4. Ruminations and Intrusive Thoughts
This type of OCD rumination is characterized by unwanted thoughts that can be difficult to control. These thoughts may be about anything, but they are often distressing or upsetting. People with ruminations and intrusive thoughts may spend a lot of time trying to suppress these thoughts or neutralize them with other thoughts.
Treatment Options for OCD
While there is no cure for OCD, several treatment options can help manage the symptoms and improve quality of life.
1. Cognitive Behavioral Therapy (CBT): CBT is a type of therapy that focuses on identifying and challenging irrational thoughts and beliefs. Exposure and Response Prevention (ERP), a specific form of CBT, is particularly effective in treating OCD. It involves gradually exposing individuals to their obsessions while preventing the associated compulsions.
2. Medications: Selective serotonin reuptake inhibitors (SSRIs) are often recommended for managing OCD. These drugs may assist in decreasing the frequency and intensity of obsessions and compulsions.
3. Other therapies: Some individuals may benefit from other therapies, such as Acceptance and Commitment Therapy (ACT) or Dialectical Behavior Therapy (DBT), which focus on acceptance and mindfulness.
Cognitive Behavioral Therapy (CBT) for OCD
Cognitive Behavioral Therapy (CBT) is a widely recognized and effective treatment approach for OCD. It aims to help individuals identify and challenge their irrational thoughts and beliefs, which contribute to their obsessions and compulsions. CBT for OCD typically involves two main components: exposure and response prevention (ERP) and cognitive restructuring.
Exposure and Response Prevention (ERP)
ERP is the cornerstone of CBT for OCD. It involves exposing individuals to their feared thoughts, situations, or objects while simultaneously preventing the associated compulsive behaviors. The goal is to gradually reduce the anxiety triggered by obsessions and learn that the feared consequences are unlikely to occur. Through repeated exposures and the prevention of compulsions, individuals can develop tolerance to their anxiety and break the cycle of OCD.
Cognitive Restructuring
Cognitive restructuring focuses on challenging and modifying the distorted thinking patterns that contribute to OCD symptoms. This involves identifying and evaluating the underlying beliefs and assumptions that drive obsessions. By replacing irrational thoughts with more rational and adaptive ones, individuals can reduce anxiety and change their behaviors accordingly.
CBT for OCD is typically conducted by a trained therapist in individual or group sessions. The duration and intensity of treatment may vary depending on the severity of symptoms. It is important to work with a qualified mental health professional who specializes in OCD to ensure the best outcomes.
Medications for OCD
In addition to therapy, medications can be an effective tool in managing OCD symptoms. While they do not cure OCD, they can help reduce the intensity of obsessions and compulsions, making it easier for individuals to engage in therapy and implement coping strategies.
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs are the most commonly prescribed medications for OCD. These antidepressants work by increasing the levels of serotonin, a neurotransmitter that plays a crucial role in regulating mood and anxiety. SSRIs such as fluoxetine (Prozac), sertraline (Zoloft), and fluvoxamine (Luvox) are effective in reducing OCD symptoms. It is important to note that SSRIs may take several weeks to reach their full effect, and potential side effects should be discussed with a healthcare professional.
Other Medications
In some cases, other medications such as clomipramine (Anafranil), a tricyclic antidepressant, may be prescribed for OCD when SSRIs are not fully effective. Additionally, antipsychotic medications may be used in combination with SSRIs or as standalone treatments for severe cases of OCD.
It is crucial to consult with a psychiatrist or healthcare provider experienced in treating OCD to determine the most appropriate medication and dosage for individual needs. Regular monitoring and follow-up appointments are necessary to evaluate the medication’s effectiveness and address any potential side effects.
Support for Individuals With OCD and Their Loved Ones
Living with OCD can be challenging, and support from loved ones can make a significant difference in an individual’s journey toward recovery. Here are some ways to offer support:
1. Educate Yourself
Take the time to educate yourself about OCD. Understanding the nature of the disorder, its symptoms, and treatment options can help you provide informed support. By familiarizing yourself with OCD, you can better empathize with your loved one’s experiences and offer appropriate assistance.
2. Be Patient and Understanding
OCD can be frustrating for both individuals and their loved ones. It is important to be patient and understanding, recognizing that OCD is a mental health condition and not a choice. Avoid criticizing or dismissing their obsessions or compulsions. Instead, offer reassurance and understanding.
3. Encourage Treatment
Encourage your loved one to seek professional help and engage in evidence-based treatments such as CBT, Interpersonal Therapy, and Medication. Weighing the benefits of Interpersonal Therapy vs CBT can be beneficial for the treatment to maximize the result. Offer to accompany them to therapy sessions or provide transportation if needed. Let them know that seeking treatment is a sign of strength and that you are there to support them throughout their journey.
4. Practice Self-Care
Supporting someone with OCD can be emotionally and physically draining. It is essential to prioritize your own well-being and practice self-care. Take breaks when needed, seek support from friends or support groups, and consider therapy for yourself if necessary.
Conclusion: Living With OCD and Finding Hope
Living with OCD can be challenging, but with the right support and treatment, individuals can lead fulfilling lives. Whether through therapy, medication, or a combination of both, there is hope for managing OCD symptoms and reducing their impact on daily functioning.
By understanding OCD’s complexities and educating ourselves about the disorder, we can foster a compassionate and informed approach to supporting individuals with OCD and their loved ones. Remember, recovery is possible, and with patience, understanding, and access to appropriate treatment, individuals with OCD can find hope and regain control over their lives.
If you or someone you know is struggling with OCD, reach out to a mental health professional for guidance and support.